![]()
This article is a part of your HHCN+ Membership
The home health industry has a high concentration of nurses that are closer to retirement age. Providers see the advantages and the drawbacks of having an aging workforce.
Broadly, the registered nurse workforce age varies based on practice setting.
In home health and hospice, the amount of nurses who are at retirement age are set to surpass new RNs, according to data from the American Medical Group Association.
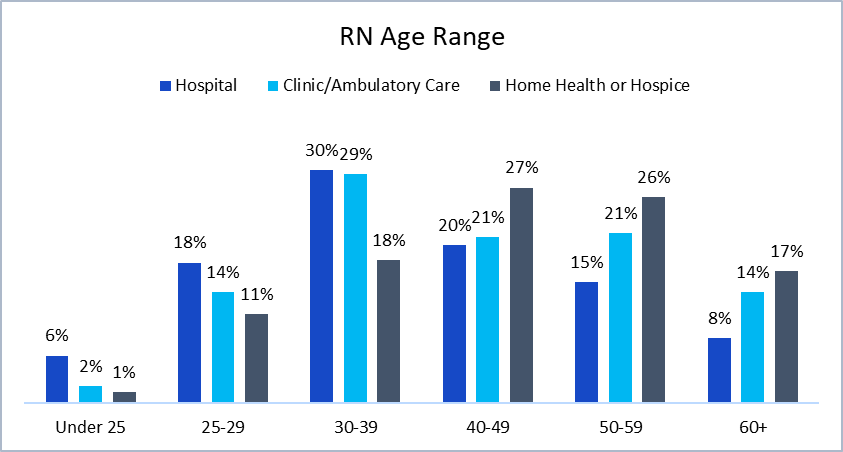
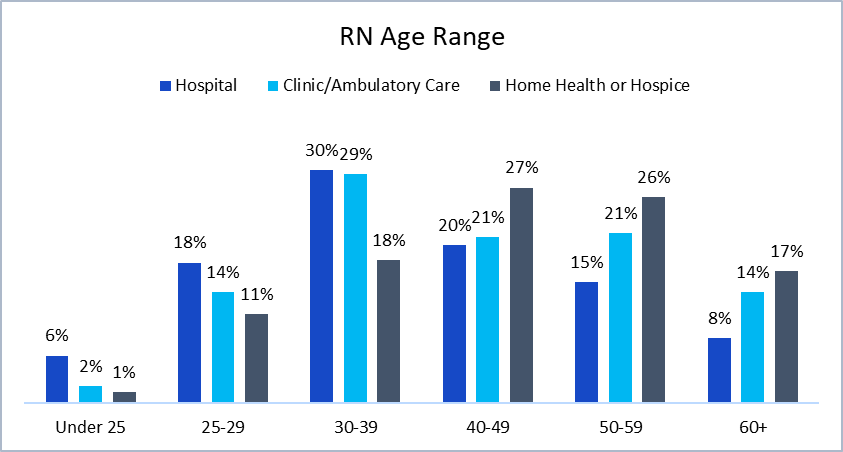 Source: American Medical Group Association
Source: American Medical Group Association
For context, the average retirement age is 63 for women and 65 for men, according to data from the U.S. Census Bureau.
One of the reasons that nurses close to, or at retirement age, make up a large proportion of the home health industry is because newly graduated nurses aren’t typically being trained to deliver care in the home while they’re in school.
“You don’t have nursing schools that are doing training in the home, it’s really focused on facility-based settings,” Katy Barnett, director of home care and hospice operations and policy at LeadingAge, told Home Health Care News. “Sometimes you’re lucky to get somebody with training in the long-term care facility space, but it’s very rare in the home.”
On the flip side, Barnett pointed out that experienced nurses are often attracted to home health care.
“We’re really looking at nurses with a lot of years of experience in other settings that come to home health, for a lot of the flexibility, but also knowing that they have that kind of clinical capacity to really serve patients on their own,” she said. “They feel comfortable and confident in serving that patient when they don’t have a clinical supervisor down the hall.”
The ability to feel confident providing care in the home is especially important because it’s a setting that calls autonomous decision making, according to Mary Carr, vice president of regulatory affairs at the National Association for Home Care & Hospice (NAHC).
“You have to make a lot of decisions independently in the home, you don’t have other nurses or clinical staff that you can grab, like you do in a hospital,” she told HHCN. “I just think it’s the preferred setting for somebody who’s a seasoned nurse.”
Another benefit of having a workforce full of mostly seasoned nurses is that they are better equipped to handle burnout, according to Barnett.
“They’ve been through a lot, and have seen a lot,” she said. “They understand the burden of the work that they’re undertaking, so the burnout rate is a little bit lower.”
At Masonicare — a Wallingford, Connecticut-based nonprofit senior care provider — 15% of nurses are over the age of 60.
“In the past year and a half, when I looked at the numbers, we actually hired four patient-facing nurses between the ages of 60 and 63,” Laurie St. John, executive director of home health, hospice and palliative Care at Masonicare, told HHCN.
As a company, Masonicare operates the full continuum of care including independent living, assisted living, skilled-nursing facilities, memory care and continuing care retirement communities (CCRCs) across three main campuses. The company also provides home health, hospice and palliative care, plus inpatient behavioral health.
St. John has noticed that working with more experienced nurses has meant less turnover.
“Our highest turnover is in first-year nurses,” she said.
Though nurses near retirement age often bring a wealth of experience to their work, there are still downsides to an aging workforce.
“You really do want people to experience the benefits of retirement, but that does lead to issues in the overall nursing pipeline, and I think that’s one of the significant drawbacks,” Barnett said.
Plus, experienced nurses leaving could mean an industry-wide brain drain of vital knowledge and history.
“Home health and home community services have really come of age in the last 20 and 30 years, so these nurses that are retiring … have been pioneers in this field,” Nicole Howell, director of workforce public policy at LeadingAge, told HHCN. “They have seen the really early stages now, the more flushed out system, and the changing needs of both the individual receiving care, and the families that are there to support them. As they move on to the next stage in their life, we’re losing not just the actual care knowledge, but really the institutional knowledge about the sector, and how far we’ve come.”
Masonicare has been able to avoid this brain drain, company-wide, as its nurses who are reaching retirement age often move into non-patient facing roles. Many of these nurses transition into educator roles that allow them to mentor other nurses at the company.
Additionally, many of these nurses who have moved away from seeing patients have played a major role in the company’s efforts to enhance its orientation process.
“We revamped our orientation process, and these nurses were critical in helping us,” St. John said. “We did focus groups with our nurses, because we wanted to hear from them — what supports you in the best way. We’ve actually added some resources to our quality and education team as a result.”