photo by McKenna Schueler
Nursing home staff and fellow 1199 SEIU union members picket outside Aspire at Rosewood in Orlando amid ongoing union contract talks (Aug. 8, 2024)
Nursing home staff in Orlando organized a picket line outside the long-term care facility Aspire at Rosewood last week, as part of a statewide action organized to raise awareness of what staff call a “care crisis.”
Eleven nursing homes were targeted. All are owned by Aspire Health Group, a for-profit company that recently acquired ownership of the 120-bed Orlando facility.
Aspire at Rosewood, formerly known as Rosewood Health and Rehabilitation, was previously owned by the mega-chain Consulate Health Care, which no longer lists facilities located in the state of Florida (save for one) after suffering years of bad press, filing for bankruptcy and going through a conveniently timed rebranding in 2022.
Staff members’ picketing action was coordinated through their union, the 1199 Service Employees International Union. The picket was organized following unsuccessful talks between the union and Aspire, which owns more than 55 facilities in the state.
Aspire and the union — including nursing home staff on the union’s bargaining committee — are currently in negotiations for a new union contract, covering over 1,000 certified nursing assistants, dietary aides and housekeepers across Florida.
Denise Allegretti, chief negotiator for the union and a former CNA herself, said Aspire’s labor relations team has put up a fight at the bargaining table, particularly on the issue of staffing levels.
“They’re refusing to even talk about staffing,” Allegretti told Orlando Weekly on the picket line, which featured about a dozen staff joined by other union members and community allies in purple union shirts, marching on the sidewalk outside Rosewood in solidarity.
According to Allegretti, “They’re [Aspire] saying they’re going to go with whatever the state says, and that’s unacceptable.” Under a Republican-backed bill signed by Florida Gov. Ron DeSantis in 2022, long-term residents of nursing homes are now only required to receive two hours of CNA care daily, down from 2.5 hours per resident.
Staff at Rosewood say this isn’t enough time to dress, feed, bathe and provide quality care for residents. They’re chronically understaffed and underpaid — many earn just a few dollars above Florida’s minimum wage of $12 an hour — leaving caregivers overstretched, frustrated and burnt out.
“We just want to give them the love that they deserve,” said longtime caregiver Diane McMullen, a CNA of 20-plus years at Rosewood. McMullen shared that she was inspired to become a CNA because of her brother, who also spent time in a nursing home. “That inspired me to become a CNA.”
Speaking of Rosewood’s residents, and the quality of resident care, McMullen stressed the importance of maintaining a workforce that’s also taken care of, and not suffering from the instability of staff turnover.
“We are their family,” McMullen said of Rosewood’s residents, as Florida’s 90-plus degree heat enveloped her and others gathered around her on the sidewalk. “We love them, too.”
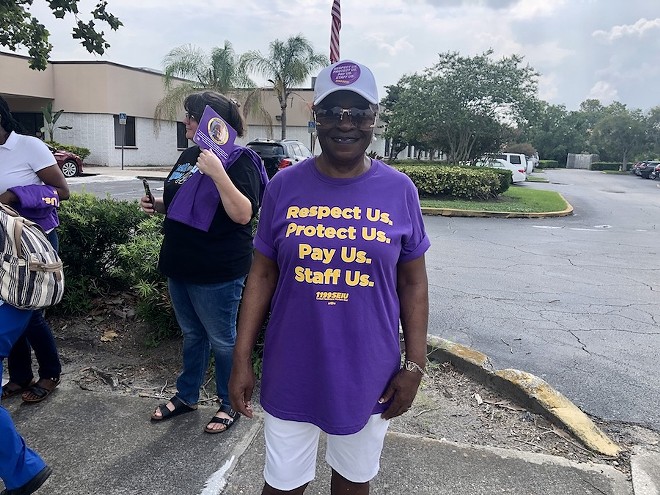
photo by McKenna Schueler
Diane McMullen, a CNA at Aspire at Rosewood and union member, pickets alongside her fellow staff and union members (Aug. 8, 2024)
Yet, when staff like herself are overstretched — tasked with taking care of more residents, with less support from their employer — they have less time to actually provide the quality of care they’d reasonably wish to provide for someone they treat as family.
This includes smaller actions like finding a resident’s favorite necklace to wear that mean a lot. “Staff don’t have five minutes to go find their necklace or their lipstick, or even give a bath on some days,” said Allegretti, the union’s negotiator.
Staffing shortages — and low pay for nursing home staff — were some of the primary issues voiced by workers Thursday, who carried signs outside of the Orlando facility demanding “Safe Staffing Now” and “Contract Now.”
“The turnover is ridiculous,” said Allegretti, clad in a purple shirt like the nursing home staff around her. “Back in the day in the ’90s, when I was a CNA, it was like eight to 10 patients on a day shift, maybe 15 on an evening shift, but never more than that,” she recalled. “Nowadays, they’re doing 15 patients on a day shift, 20 or more on a night shift, which is criminal.”
According to federal data compiled by ProPublica, nursing homes owned by Aspire Health Group in Florida have seen a higher-than-average rate of “serious deficiencies,” and higher-than-average staff turnover.
A federal inspection report, published in April, found over a dozen deficiencies in the Rosewood facility’s operations in Orlando, all posing “no harm, but with a potential for more than minor harm,” according to inspectors.
Deficiencies identified ranged from quality of care issues, such as failing to provide trauma-informed or culturally competent care, to pharmacy issues, like medication errors.
“We just want to give them the love that they deserve,” said longtime caregiver Diane McMullen, a CNA of 20-plus years at Rosewood.
tweet this Under different ownership, the facility in 2022 was fined $163,183 over three severe deficiencies identified by inspectors, posing an “immediate jeopardy to resident health or safety,” and two deficiencies posing minimal or no harm.
Some of Aspire’s other facilities in Florida have similarly been cited for deficiencies, including inadequate supervision at Aspire at Saint Lucie on the Treasure Coast and a failure to “[E]nsure that a nursing home area is free from accident hazards,” according to an April report summarizing deficiencies.
Aspire Health Group has faced an average fine of $50,782 in penalties for health citations, according to the ProPublica database. Penalties are issued by the Centers for Medicare and Medicaid Services for serious health citations, or for health citations that have not been fixed.
As The New Yorker reported in 2022, federal staffing rules haven’t changed for nursing homes since 1987. In April of this year, the Biden-Harris administration took action to change that, announcing a new rule on minimum staffing standards in nursing homes that will, for the first time, establish minimum staffing requirements in such facilities overseen by the Centers for Medicare and Medicaid Services.
The implementation of this new rule, however, is subject to a “staggered implementation timeframe,” according to CMS. The union in Florida argues that “immediate and contractual obligations for safe staffing” are needed from nursing home operators in Florida now — not later.
“Staffing and retention always has been an issue because it can be a complicated and back-breaking job for very little pay,” said Margarette Nerette, vice president of the union’s Long-Term Care division, in a recent statement.
“Add the pandemic where workers were at ground zero of COVID risk, lowered safe-staffing rules in Florida, and the state’s skyrocketing housing and insurance costs, and we have a perfect storm of pressure,” Nerette continued. “To help relieve this crisis and to better protect patients and their caregivers across the state, we’re fighting for new contracts that respect us, protect us, pay and staff us.”
The workers’ fight for a fair contract — and meaningful action on the issue of staffing — comes in the wake of a financial boost approved for nursing home operators by the Florida legislature and Gov. Ron DeSantis earlier this year. As part of the state’s 2024-25 fiscal year budget, state leaders approved a $247.8 million Medicaid increase for the state’s nursing home operators, in part to help address staffing problems.
“The state budget provides an 8% increase ($247.8 million) in Medicaid funding, amounting to nearly $470,000 per center, per year to support the state’s nursing centers with meeting the growing demand for qualified caregivers and the needs of Florida’s vulnerable seniors and people with disabilities,” the Florida Health Care Association shared in a statement celebrating the extra funding.
The Florida Health Care Association, a state affiliate of the nation’s largest nursing-home lobbying group, represents over 86 percent of Florida’s nursing centers — with Aspire-owned facilities among their federation’s membership.
Aspire Health Group facilities in Florida have, as part of their membership, contributed to the FHCA’s political activities through regular contributions to an associated FHCA PAC. State records show Aspire facilities have contributed over $20,000 to one of their PACs in 2024 alone.
Getting a fair union contract for staff at Aspire-owned nursing homes would give residents “a better home,” said CNA McMullen. “A better home for them, better staffing and better wages for us,” she added.
Registered nurses at HCA Hospitals in Florida have similarly raised alarms about unsafe staffing levels at their facilities, and are also in negotiations for a new union contract.
Nurses at HCA Osceola Hospital, represented by National Nurses United, organized their own picket line on Thursday, calling on their multi billion-dollar, for-profit employer to invest in high quality staff and patient care.

photo by McKenna Schueler
Nursing home staff and fellow union members picket outside Aspire at Rosewood, a nursing home in Orlando (Aug. 8, 2024)
“We’ve been at the bargaining table for months fighting for what we need to take care of our patients,” said Elisabeth Mathieu, a registered nurse in HCA Osceola Hospital’s emergency department, in a statement. “We need HCA to hear us, so we’re holding this informational picket to let the public know what we’re demanding in our contract when it comes to patient care and, especially, safe staffing.”
The most recent NNU contract covering RNs at 10 HCA hospitals in Florida — including HCA Osceola and HCA Lake Monroe in Sanford — was negotiated in 2021. The contract officially expired July 1, after being extended once from its original May 31 expiration date.
The union contract covering nursing home staff at Aspire Health Group facilities, represented by 1199 SEIU Healthcare East, has also expired, according to Allegretti.
Nearly 50 nursing home facilities in Florida represented by 1199 SEIU Healthcare East, covering 4,000 staff total, have union contracts that have expired or will expire at some point this year, according to the union.
While NNU staff have politely declined to comment on what the next steps are for RNs that they represent, if HCA continues to remain resistant at the bargaining table, Allegretti said that if Aspire Health Group fails to budge, the next step for their union is a strike vote.
“If management doesn’t follow us with [bargaining] dates, and come with real proposals, the next step is that we will be out on strike,” Allegretti confirmed.
The last time workers went on strike at the Rosewood facility in Orlando, and 18 other nursing homes in Florida, was 2016. The union described it then as the largest-held strike in the Southeastern United States in nearly two decades.
Subscribe to Orlando Weekly newsletters.
Follow us: Apple News | Google News | NewsBreak | Reddit | Instagram | Facebook | Twitter | or sign up for our RSS Feed




:max_bytes(150000):strip_icc()/Update-Pull-and-Push-Day-Workout-d3bbeb169bae427a99dd5162993f6641.jpg?w=360&resize=360,270&ssl=1)