The share of skilled nursing leaders reporting flexible scheduling initiatives jumped significantly in 2024, reflecting the lengths employers have gone to to improve recruitment and retention.
But the looming federal staffing mandate is already being viewed as a threat to the sector’s newfound, delicate appreciation for work-life balance.
More than half (55%) of the administrators and nurse leaders responding to the 2024 McKnight’s Mood of the Market survey said they do not believe the mandate will improve their personal workload once fully implemented.
That share was at about half (49.5%) among nurse leaders, many of whom commented that they expect to be pulled into unwanted overtime shifts or become reliant again on agency nurses if their facilities cannot find enough registered nurses to hire. The mandate requires all non-rural nursing homes to have an RN onsite 24 hours of every day starting in May of 2026.
“It is harder and harder to find competent staff to replace staff that leave,” noted one anonymous participant, who joined others in noting the higher wages hospitals can afford to pay RNs. “I believe it will become an issue sooner than we realize.”
This year’s Mood of the Market survey drew 723 responses from directors of nursing, assistant directors of nursing, administrators and their assistants. It was distributed by email from late July to mid-August.
Thousands fearing closure?
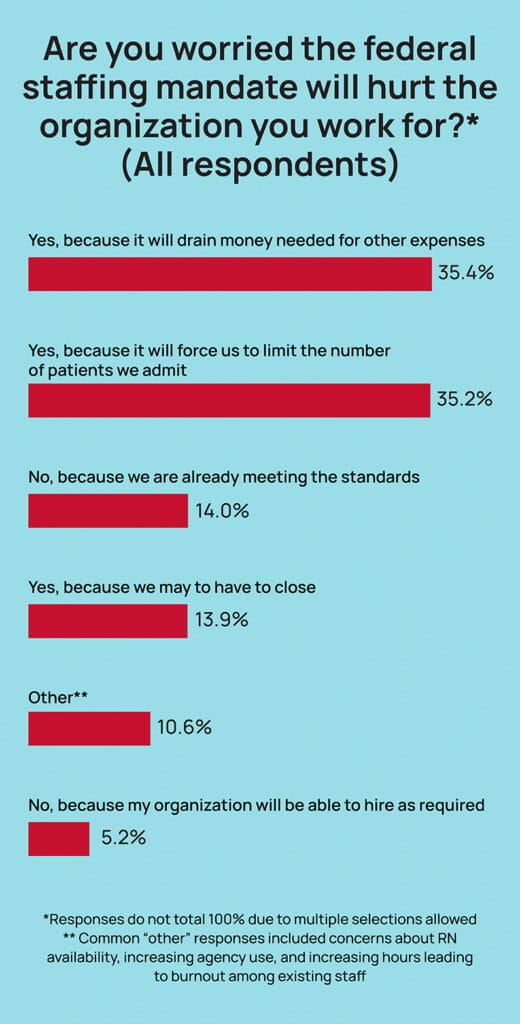
While 22.5% of nurses and 20.7% of administrators do believe the mandate will improve their personal workload, almost all respondents expressed concerns about the potential effects on their organizations.
Some 35.4% said the mandate will hurt the organization they work for because it will drain money needed for other expenses. Another 35.2% said it will “force us to limit the number of patients we admit.”
Another 13.9% said the mandate may force their facility to close.
Extrapolating that to all 15,000 or so US nursing homes should give anyone involved in staffing or regulating the industry reason to pause, said Mark Prifogle, chair-elect of the American College of Health Care Administrators.
“We’re talking about 2,000 communities, and let’s say 213,000 residents that could be affected,” said Prifogle, vice president of operations at BHI Senior Living, with 10 life plan communities in Indiana, Michigan and Ohio. “Anytime new regulations come into effect, there are some people who will go to the extreme with their concerns. Here, we know we want to comply. But for many providers, even if we have the money to pay them, there are not enough nurses in the healthcare ecosystem.”
And Prifogle says he and other administrative leaders are already wondering how well RNs will hold up if forced back into a COVID-era routine of taking on extra shifts they may not want so their employer can avoid penalties.
“You’re going to leverage the RNs you have until they leave,” said Prifogle, noting the lack of federal mandates for other settings. “Even the people that want overtime, when you do that for 10 weeks in a row, that’s tough.”
That fear of a new turnover cycle in their buildings may be one reason administrators were even more likely than nurses to say the mandate would not improve their personal workload. Nearly 60% said it would not.
Providers tout flexibility muscle
Concerns about the mandate’s effect — and regulatory burden, more generally — were among the relatively worrisome findings in this year’s Mood of the Market survey.
A smaller percentage of employees said they had been thinking about quitting, and more said they were “very satisfied” with their jobs, compared to the 2023 Mood survey.
Still, nearly 100 respondents still told McKnight’s Long-Term Care News a more flexible schedule would be one of two changes that would most improve their job satisfaction. Among nurses, 14.5% chose that option, with 16.7% of administrators selecting it.
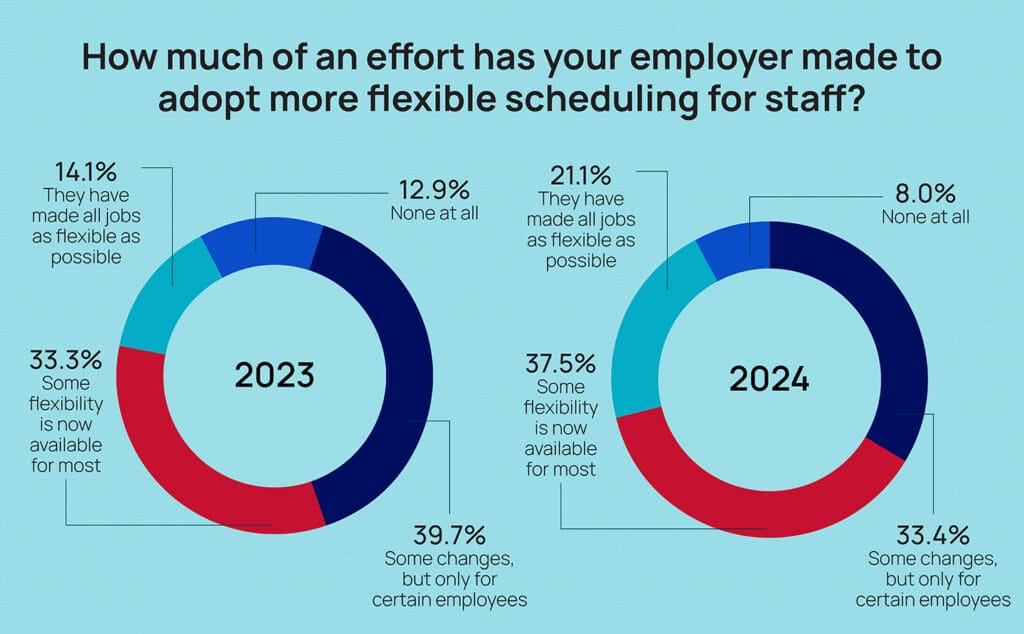
That’s despite 58.6% of all respondents saying their employer had created more flexibility for most employees, or made all jobs as flexible as possible. That was up significantly from 47.4% in 2023.
Respondents said they were most likely to have more part-time opportunities (43.4%), three- or four-day workweeks (42.9%) and the ability to self-schedule (30.5%).
Many respondents noted under an “other” option that their employers are offering less formal types of flexible scheduling, such as time off to attend children’s activities, trading hours with colleagues, creating more flexible weekend options, and allowing some remote work for administrative staff.
Denise Boudreau, president of Drive, said employers’ increasing willingness to accommodate requests for understanding in unique situations — or being open to program a variety of schedules — has gone a long way toward keeping valuable employees in the sector.
“For the most part, people know they’re in a 24/7 field,” said Boudreau, whose company helps senior care organizations assess and improve workplace culture.
”When people are talking about work-life balance, they get the fact that they’ve got to work a weekend or a holiday. I think real work-life balance is, what does it particularly mean to that person? Can I go to the Mother’s Day lunch? Could I get out at a time earlier than 5:00? The key is the flexibility is there when you need flexibility.”
Carrying that burden
One place most employees won’t find flexibility is with regulatory agencies.
This year, nurse leaders — those most often tasked with completing daily regulatory requirements as part of their workflow — had a clear target for their annoyance.
“Adoption of enhanced barrier precautions” by the Centers for Medicare & Medicaid Services this spring was the No. 1 regulatory or payment change to add burden to nurses’ jobs this year, according to the survey. Some 25.6% of nurses chose the option, which was followed by “increased CMS Quality Reporting requirements” at No. 2.
Amy Stewart, chief nursing officer for the American Association of Post-Acute Care Nursing, said that ranking was not a surprise “at all,” given continued questions about when exactly to use the precautions.
“The new verbiage about close contact [precautions] is subjective. You don’t need it in the dining room, but that transfer might be as long as another activity and then you need it for that. I think it’s very confusing,” Stewart told McKnight’s. “The other thing is there’s the volume of people requiring it. One day, we didn’t use enhanced barrier precautions on them and the next day, we did. It’s for the safety of the residents and staff. But the residents don’t understand why we’re doing this either.”
Providers are also absorbing extra costs for gowns and gloves, plus the added time it takes staff to ensure requirements are followed to regulatory standards, Steward noted.
Ongoing issues with the recent MDS changeover also continue to be the top regulatory complaint of 15.9% of nurse respondents. Stewart suggested that could be tied to problematic differences between state and federal reporting requirements, which could worsen as more states adopt their own case mix indexes for Medicaid reimbursement.
Respondents also repeatedly sought regulatory relief across open-ended responses available on multiple questions this year. As for what would most improve job satisfaction, 10 of 60 “other” responses addressed burdensome government requirements.
“Reporting requirements and survey/survey-related tasks consume too much time,” one respondent wrote. “More time should be available to focus on residents, families and staff.”
This is the third article in a four-part series. Previously, we explored long-term care’s quitting problem — is it going away? — and pay satisfaction. Next week, we examine what skilled nursing leaders optimistically say is going right in their workplaces.




