Study design
The study was an interventional evaluation study with a before-and-after comparison conducted over three years’ duration starting from Jan. 2017 till Jan. 2020. A quasi-experimental design with posttest-only control design was done. Two villages were included in the study as intervention and control villages. This design was chosen to prevent possible contamination if the other village was chosen as a control before the intervention so that the real impact could be assessed.
Study setting and participants
The intervention village
El Othmanyia village of El Mahallah El Kubra district– Gharbyia governorate was selected as the site of the project implementation. El Othmanyia village total married women in the childbearing period (19–45 years) were 2100. The control village was chosen as a matched group from the control village (Nemra el Basal village). The Economic Research Forum and CAPMS in Egypt have developed a wealth index that is based on the socio-economic status and was used for the classification of the socioeconomic status of the villages [32, 33]. Using the human development index, both villages were selected from the same governorate and the same district to have the same sociodemographic status, but in different local village unit (one in the east and the other in the west of El Mahallah El Kubra district) to have similar socioeconomic status.
The selected villages have powerful and active well-organized community-based associations with on-ground community health workers (CHWs) who were trained and serve as key players for the provision of motivational messages to the target groups.
Target groups
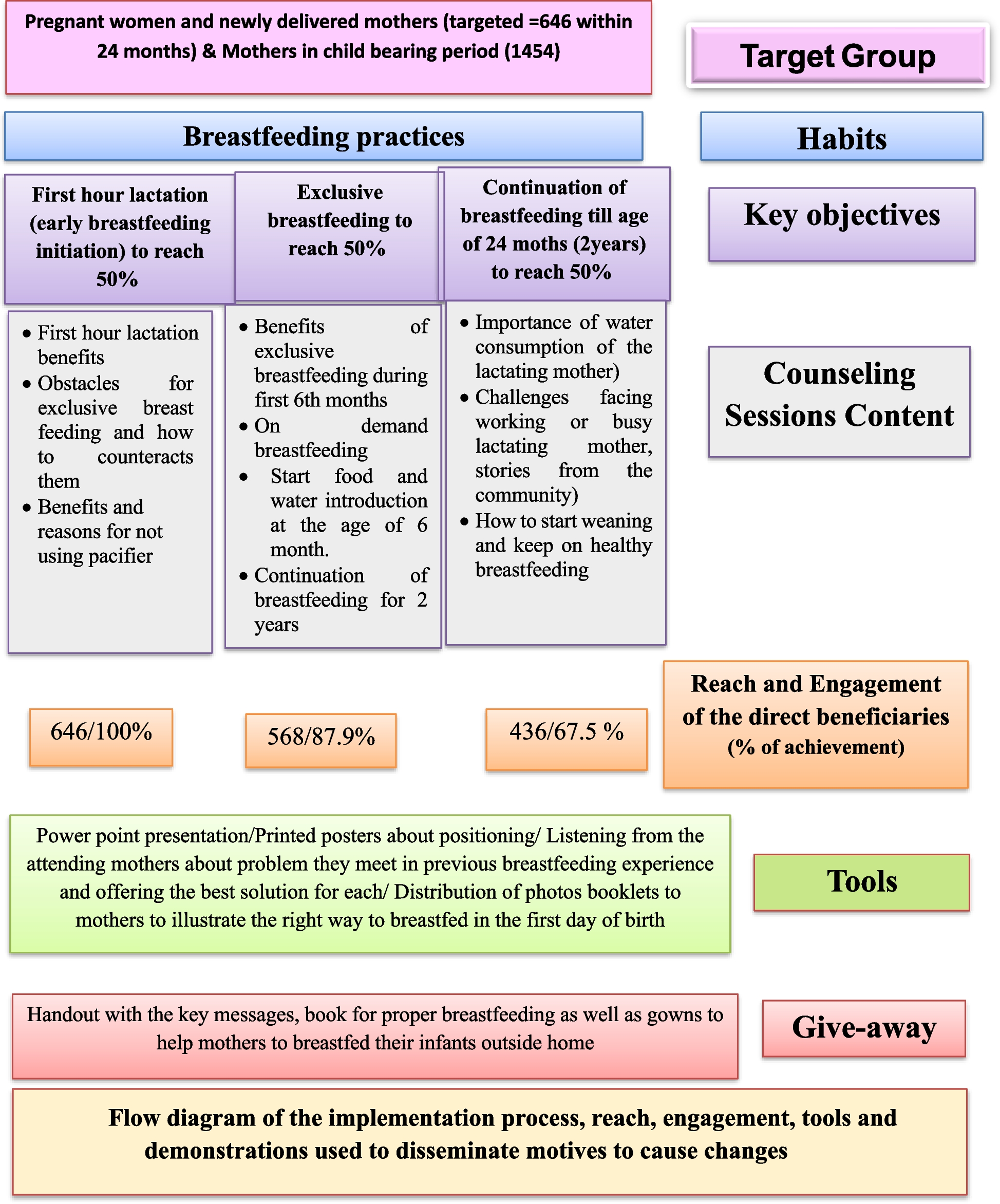
The direct beneficiaries for the intervention included pregnant women in their third trimester to help them have the best start and initiate their breastfeeding as soon as possible after birth, as well as mothers of newly born (at birth). Accordingly, a total of 646 mothers of infants were enrolled in the study along 2 years of follow-up. Women in their childbearing period (future mothers) were also targeted as indirect beneficiaries (n = 1454). A total number of 2100 women, including women who intended to breastfeed their infants and those who did not and who signed informed consent forms, were targeted for the intervention. The age range of the women enrolled in the study was 19–45 years. The total number of mothers who engaged in the study were those who completed the intervention sessions; completed the 10 messages within three months of the interventions and engaged in the quarterly follow-up visits within two years of intervention (Fig. 1). Engaged mothers were 436 out of 646 enrolled (67.5%).
Fig. 1
Flow diagram of the implementation process, reach, engagement, tools and demonstrations used to disseminate motives to cause changes
Phases of the study
The study was conducted in phases; the first was the formative assessment research followed by the interventions phase and ended with evaluation for measuring the outcome and impact.
Phase one; assessment phase
Participant in-depth interviews and formative research were used to collect data from the beneficiaries. The in-depth interview focused on listening to the attending mothers about problems they met in their previous breastfeeding experience and offering the best solution for each. Community consultation to help identify the “Best practices”, those appropriate, convenient, and suitable with the local culture and capabilities was also conducted. Meanwhile, formative research was used to assess the current situation of breastfeeding practices and identify the behaviors to be targeted, pricing, and promotional messages. The formative research also identified the factors that influenced mothers’ decisions to breastfeed and those that hindered or encouraged women to breastfeed. All practices were determined according to the designed pre-tested questionnaire.
Phase two; intervention phase
The interventions included capacity building of the activities’ implementers by the research team specialists from the National Research Center of Egypt which lasted for 4 months. The training was directed to 7 community health workers (CHWs); 5 nurses and 2 physicians of the rural health unit of the intervention village. So that they became community educators delivering the right messages about proper breastfeeding practices to all participants. They were targeted by the educational toolkit developed by the related researchers which was tailored more specifically to their needs and respected their norms according to the findings of the assessment phase.
Health education and counseling interventions targeted both the direct and the indirect beneficiaries. The longitudinal interventions followed over 646 mothers from early pregnancy throughout their infant’s second year of life.
Counseling sessions related to the importance, early initiation, and continuation of mothers to successfully breastfeed their infants and identifying the warning signs that need breastfeeding consultant intervention were delivered over 12 months to target the primary beneficiaries. For each mother 10 messages that are related to the targeted breastfeeding indicators for change [1] were delivered over 3 months; 3 messages were covered in the first session during the first month and 4 messages were added and covered in the second session during the second month and 3 different messages were added during the third session during the third month. Then, this is followed by repeating the same messages every 3 months. Accordingly, during 12 months of implementation, 4 rounds were conducted to cover delivering the messages to all targeted participants. Concerning the direct beneficiaries, the first set of messages was attended by 646 pregnant and delivered mothers. The second set of messages was attended by 568 mothers, and the third by 436 mothers. The activation process for the targeted primary and secondary groups with follow-up was conducted quarterly for 24 months for each mother. The flow diagram of the educational interventions’ implementation process, messages, reach, engagement, tools, giveaways, and demonstrations used to disseminate motives to cause change, is illustrated in Fig. 1.
Pregnant women and newly delivered mothers who were reached were 646 of which 436 were engaged in the counseling sessions and were covered by all messages for 24 months with an engagement rate of 67.5% (Fig. 1). The major reason for the dropout is the engagement of women in household and fieldwork activities.
The interventions were based on the use of a social marketing approach. This approach was based on using the motives for successful breastfeeding practices and overcoming the detected obstacles and factors contributing to declining of breastfeeding practices for improving breastfeeding practices over one year of interventions. A set of interventional messages concerning proper weaning practices was directed to our beneficiaries and its results were published [34].
Phase three; evaluation phase
Two methodological approaches were used during the evaluation; the first was by comparing the conducted practices as a result of the intervention between the intervention villages with those who did not receive any intervention in the non-intervention village. The second was through looking for direct evidence: Assessing the change in breastfeeding practices as well as the growth before and after the interventions within the intervention village which means that the study group served as self-control.
The end-of-study evaluation was done once the interventions had been completed through using a participatory approach by CHWs under the supervision of the study team. To measure the intervention’s effectiveness, mothers and their infants were assessed and evaluated by the same structured questionnaires to test the breastfeeding practices and infants’ growth before and after the interventions.
Basis for sample size calculation during the assessment and evaluation phases
A sample size of 141 houses produced a two-sided 90% confidence interval with a width equal to 0.100 when the sample proportion for exclusive breastfeeding up to 6 months of age is 0.130 [14] which was rounded to 150 households [35, 36]. Houses were randomly selected out of the houses of the direct beneficiaries who engaged in the intervention (n = 436 mothers). Houses were selected by a systematic random sample. A total number of 200 women who were residents in these houses and who fulfilled the selection criteria were enrolled in the assessment and evaluation stages together with their infants aged 6 months up to 12 months. All infants of eligible mothers were included (one or 2 infants). For the rest of the mothers who were enrolled in the study (210 of 646 mothers) but did not engage in completing the intervention, their initial data were discarded, and they were excluded from being evaluated.
Confidence interval formula: exact (Clopper Pearson)
|
Confidence Level |
Sample Size (N) |
Target Width |
Actual Width |
Proportion (P) |
Lower Limit |
Upper Limit |
Width if |
|---|---|---|---|---|---|---|---|
|
0.900 |
141 |
0.100 |
0.100 |
0.130 |
0.086 |
0.186 |
0.145 |
Key Performance Indicators (KPIs):
The core KPI which are the study primary outcome to evaluate the success of the interventions were defined according to the World Health Organization, 2019 [37]:
-
1.
Early initiation of breastfeeding
-
2.
Exclusive breastfeeding (EBF) under 6 months
-
3.
Continued breastfeeding at 1 year
-
4.
Continued breastfeeding at 2 years
-
5.
Children ever breastfed
-
6.
Predominant breastfeeding under 6 months
-
7.
Bottle feeding with formula
-
8.
Percentages of responsiveness to cues of hunger and satiety
Exclusive breastfeeding: The infant has received only breast milk from his/her mother or a wet nurse, or expressed breast milk, and no other liquids or solids with the exception of drops or syrups consisting of vitamins, mineral supplements, or medicines [1].
Predominant breastfeeding “allows” Oral Rehydration Salts (ORS), vitamin and/or mineral supplements, ritual fluids, water and water-based drinks, and fruit juice. Other liquids, including non-human milk and food-based fluids, are not allowed, and no semi-solid or solid foods are allowed [1].
Interventions targeted the control group within the control village were social by design
The well-trained community members who were the local people engaged in the implementation process of the intervention village, act as educators for the social workers of the control village. Such engagement was a social dynamic that fostered continuous engagement which worked towards sustainability and the continuation of the process resulting in lasting and continued positive behavior change. All participants from the control village received the educational toolkit developed for promoting breastfeeding practices as well as the giveaways (Fig. 1).
Social marketing (SM) approach
Health education through using social marketing principles [29]: The implementation of the market plan focused on increasing the reach and engagement of mothers to have a profound impact and sustained success of breastfeeding. The marketing plan included the following:
Target behaviors (outcome)
-
1.
Increase breastfeeding early initiation rates
-
2.
Increase breastfeeding duration rates to 2 years
-
3.
Increase the rate of EBF under 6 months
-
4.
Increase general public support for breastfeeding practices
Product(s)
The Product is breastfeeding. The choice of breastfeeding benefits that has been emphasized was identified during formative research according to each targeted behavior.
The formative research indicated that the emotional benefits to the baby were emphasized more than the health benefits be more influential with mothers.
Price
For addressing the price factor, the marketing plan focused on interventions to lower the identified costs (barriers to breastfeeding and faulty beliefs) or make them more acceptable.
Encouragement of responsive feeding of mothers to their babies’ cues of hunger and satiety is free of charge. The following guiding principles during breastfeeding were provided and all are free of charge; feed directly or assisted, feed slowly and patiently, encourage feeding without forcing and avoid distractions while talking and looking at the child.
Moreover, behavioral change through the SM approach was applied to overcome the identified barriers by teaching the health providers to increase the awareness and concern of the mothers of breastfeeding’s motives (benefits) and help mothers develop ways to lower the costs (barriers) most relevant to them personally.
Place
The Place factor was addressed by using the governmental public health facilities (the village rural health unit) and the village community-based associations to make these public settings more welcoming to breastfeeding women. Moreover, nursing women were also reached at their homes through the CHWs.
Interventions to facilitate support for breastfeeding practices through professional training directed towards nurses, physicians, and health workers at the rural health unit as well as the village community-based association’s members so that they could discuss breastfeeding with family members and friends.
Promotion and motives
The promotional messages targeted factors detected to motivate and deter from encouraging women to breastfeed. The promotion messages used were out of the reported motives by ever breastfed mothers (190 mothers) that were expressed by more than half of the mothers; mainly: Save money, time, and effort, increase the mother-baby bond, and boost the child’s immunity. In addition, reasons for not using the pacifier were also added to the motives.
Slogan
The slogan of promotion to breastfeeding “feed me like a baby” was used for message distribution. The messages were converted to posters and cards. The content of the message although being derived from the women themselves and socially responsive was tested through 4 focus group discussions each with 10 women. The four selected focus groups were: Pregnant women, mothers of infants 0–6 months, mothers of infants 6–24 months, and women in the childbearing period.
The messages were from babies to their mothers “One thing I wanted to tell you, my mom, once I’m out feed me like a baby. Breastfeed me for the 1st 6 months, and don’t give anything else before I’m 6 months, continue breastfeeding me for up to two years. The only food I will love is the one coming from you. When you breastfeed, me you will not only save money, time and effort but also increase my immunity. I feel you and you feel me in your heart, please do not use the pacifier as it makes me vulnerable to infection. LOVE you, mom.”
Change support process
Some tactic points were used to support the SM approach through:
-
The village’s pediatricians were requested to encourage breastfeeding over other substitutes while providing recommendations for the mothers
-
Nurses were trained to help mothers on how to start and overcome the initial challenges of breastfeeding.
-
Distributing maternity messages on breastfeeding tips for moms who have Android mobiles using the WhatsApp application.
-
Mothers were introduced to the competition, those who joined the competition received free breastfeeding covers (gown) to encourage them to breastfeed in public.
Methods
A well-structured questionnaire was applied to the target groups through an interview to collect the nutritional data. The Centers for Disease Control (CDC) Infant Feeding Practices Questionnaire [38] was used to measure feeding practices throughout the first year of life. The main topics covered in the questionnaire included: Food fed to the infant, including breast milk and infant formula, patterns of breastfeeding, solid food intake, and other complementary foods and liquids were recorded. In addition, the timing for initiation of breastfeeding, the duration for exclusive breastfeeding or predominant breastfeeding or bottle feeding with formula, and the responsiveness to cues of hunger and satiety were also assessed and evaluated. Moreover, factors that may contribute to infant feeding practices and breastfeeding success and other issues (e.g. experiences with breast pumps and pacifiers) were also investigated.
Growth assessment was done for each infant aged 6–12 months twice (before and after the interventions) using anthropometric parameters.
All anthropometric measurements were taken by using standard anthropometric protocols and standardized instruments. Z scores (WAZ, HAZ, and WHZ) were calculated for each infant. They were measured, following the recommendations of the “International Biological Program” [39]. Infant Body Mass Index (BMI) was calculated: weight (in kilograms) divided by height (length) (in meters squared). The infant’s BMI percentile was calculated for age and sex based on the Egyptian Growth Reference Charts [40]. The standard deviation score (Z score); to exclude the effect of age; was calculated for the weight (WAZ), height (HAZ), and BMI (BMI-Z) according to the Egyptian Growth Curve by the following equation [41].
$$mathrm{Z ,score}=frac{{{text{individual}}}^{mathrm{^{prime}}}mathrm{s ,variable}-mathrm{ mean ,value ,of ,reference ,population ,SD ,of ,the ,reference ,population}}{mathrm{SD ,of ,the ,reference ,population}}$$
The researchers, who are anthropologists, took anthropometric measurements on the infants, including weight, supine length, occipitofrontal circumference (head circumference HC), and mid-upper arm circumference (MUAC) on the left arm. A flexible, non-stretchable measuring tape was applied to assess measurements to the nearest 0.1 cm, following standardized research protocols and Quality control measures elaborated for the World Health Organization Multicenter Growth Reference Report [42]. Each infant was also examined by the Holtain Body Composition Analyzer (Computerized Holtain Body Composition Analyzer -Holtain’s BCA, Holtain Ltd., UK, Wales, Crosswell No.646512). The following parameters were derived: the percentage of body fat (Fat %: an estimate of the proportion of fat to the total body weight), fat mass (FM: an estimate of the fraction of the total body weight that is adipose tissue), fat free mass (FFM: an estimate of the fraction of the total body weight that is not adipose tissue) [43] and Total Body Water (TBW: an estimate of the fluid occupies intracellular and extracellular spaces, comprising about 0.6 L/kg (63.3%) of body mass) for hydration assessment [44, 45].
Data quality assurance
Data quality was controlled through condensed training sessions about how to conduct the questionnaire in a standardized way given to the data collectors. Data collection was conducted under the supervision of professional team members from the National Research Centre of Egypt (NRC) and their appropriate supervision that was carried out by the National Research Centre team members. A pilot study was performed on 10% of the questionnaire to ensure the validity of the questionnaire items by revising and modifying difficulty-understood items or language and then re-introducing them. The results of the pretest were not included in the study.
Setting targets for the interventions
According to the assessment results, the target objectives were set to be realistic and achievable as follows: For any of the studied breastfeeding (BF) indicators, if its measure was 25% or less, the target was set to reach 50%. For any indicator whose measure was in the range of 25- 50%, the target was set to reach 75%. For any indicator whose measure was > 50% and < 75%, the target was set to reach 70–80%. For any indicator whose measure was > 75%, the target was at least to sustain the indicator.
Statistical methods
After data cleaning, all completed questionnaires were entered into the computer. Statistical analysis was done by using the Statistical Package of Social Software program (SPSS), version 26. Data were presented as quantitative and qualitative variables. The quantitative variables included: the mother’s age, the number of children in the house, body circumferences, and body composition parameters. The qualitative variables included: the mother’s education, occupation, marital status, awareness of the meaning of exclusive breastfeeding and its benefits, awareness of initiating breastfeeding during the first hour of delivery, awareness of the meaning of colostrum milk and its benefits, intention of start weaning, intention of continued breastfeeding, consumption of liquids in the first day of delivery and among children < 6 m, consumption of solid, semi-solid or soft food among children < 6 m, breastfeeding and bottle feeding, breastfeeding during illness, breastfeeding initiation during the first hour of delivery, exclusive breastfeeding under 6 months, continued breastfeeding, frequency of breastfeeding per day, children ever breastfed, WAZ, WLZ. For quantitative variables, the data were summarized using descriptive statistics, where mean and standard deviation were used. However, numbers and percentages were used for qualitative values. Before and after the intervention, related indices were compared for the studied group. The following tests of significance were used: Pearson’s Chi-square test (χ2) and Z test (for qualitative data), paired t-test (for continuous data between the pre and post-interventions), and t-test (for continuous data between means of two groups). Percent change or mean change was measured for the differences between pre and post-intervention, where + ve good indicator or -ve bad indicator means improvement in these indicators and vice versa. A P-value less than 0.05 was considered statistically significant, while a P-value less than 0.01 was considered highly statistically significant.