When it comes to their mental health and well-being, home-based care aides are susceptible to stress and depressive symptoms due to working conditions, a new study from Weill Cornell Medicine researchers found.
To compile this study, focus groups and interviews with home-based care aides were conducted from August 2022 to February 2023, in partnership with the 1199SEIU Training and Employment Fund.
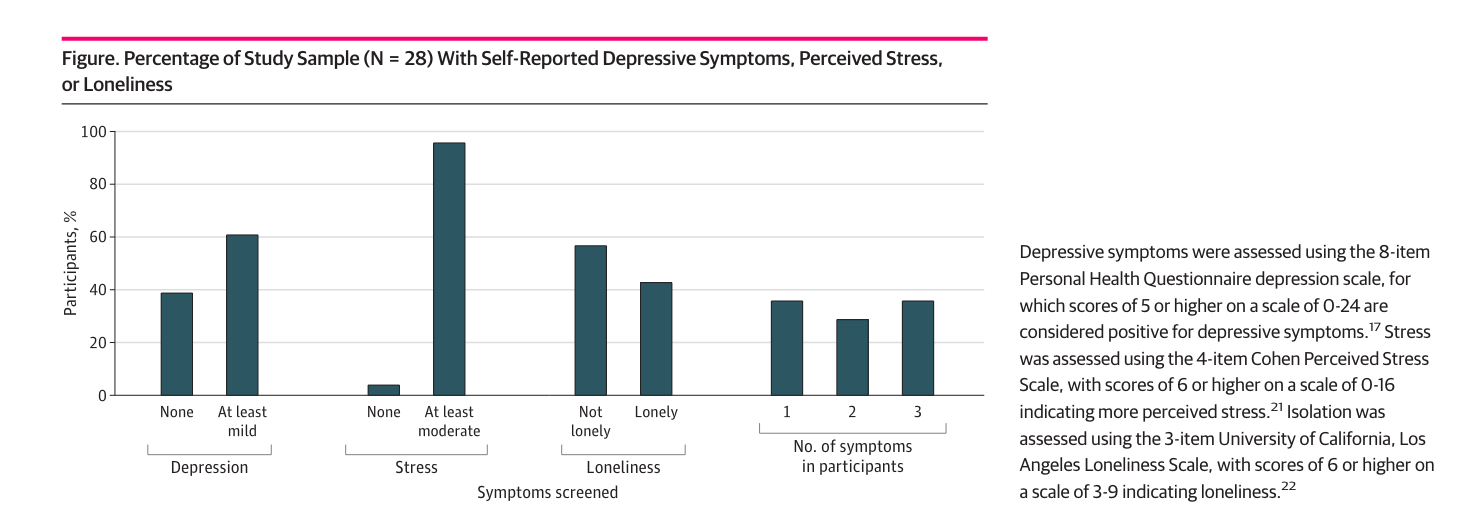
Interview and focus group participants included aides who had at least mild or more symptoms on either the 8-item Personal Health Questionnaire depression scale, the 4-item Cohen Perceived Stress Scale, or the University of California, Los Angeles, Loneliness Scale.
Many key findings were revealed through the study, including that personal and cultural factors impact aides’ outlook toward mental health.
“While some participants reported feeling comfortable with discussing their mood, others reported stigma around mental health, which made it challenging,” researchers wrote in the study. “One participant said that ‘a person mentions something about mental health, then it crosses your mind that this person may … have mental problems.’ The first thing you think is, ‘They’re crazy. … It makes you feel ashamed or afraid.’ In general, personal responsibilities outside of work, including family caregiving, affected their mood.”
Another important finding was that aides’ relationships with their patients can influence their moods.
The study noted that caring for patients that require services beyond the agency’s plan of care was particularly challenging.
On the flip side, forging meaningful relationships with their patients could be gratifying for aides.
Structural and organizational aspects of the job, as well as the COVID-19 pandemic, were also found to be stressors that impacted mood.
“Many described that working extended hours, having long commutes and receiving inadequate compensation substantially impacted their well-being,” researchers wrote.
Plus, some participants expressed that they were experiencing difficulties with their home care agencies, which added to their stress, including things like poor communication and insufficient information about patients.
Researchers also sought to learn how aides were coping with stress and depressive symptoms. They received a range of responses.
“Many discussed doing breathing exercises and meditation, engaging in prayer, and physical activity,” researchers wrote. “As one participant explained, ‘The first thing I do is pray to God to give me strength to move forward because the struggle here has not been easy.’ Additional strategies that participants reported using included listening to music, watching TV, playing games, reading and taking courses. One participant said, ‘Sometimes I try to hide it, but I do cry. But then afterwards, I try to calm down a bit. I don’t know, sometimes I play music. I entertain my mind.’”
Ultimately, many of the study participants called for programs that could help them. Participants suggested courses on mental health, or wellness should be made available through their union or home care agencies.
Some also suggested that peer coaching could be a helpful resource.
“The need for on-the-job support from other HHAs was also driven, in part, by participants’ expressed difficulty in discussing their professional experiences with their families,” researchers wrote. “The reasons they cited were concerns about patient privacy or their preference to keep work and family life separate.”



