Listen to this article
As part of NJBIZ’s latest virtual discussion, health care executives in New Jersey spoke about current trends in technology, practice and policy as it relates to their industry. Moderated by NJBIZ Editor Jeff Kanige, the Sept. 24 panel featured:
- Karen Lindgren, chief clinical officer at Cherry Hill-based Bancroft, one of the state’s largest nonprofit providers of services for people with autism, intellectual and developmental disabilities, as well as individuals with brain injury and neurological conditions.
- Jennifer D’Angelo, chief operating officer & executive vice president of healthcare at New Jersey Innovation Institute.
- Said Haddad, president of J&J MedTech Surgery, a Johnson & Johnson subsidiary that makes medical devices.
- Patrick Young, president of population health for Hackensack Meridian Health, the most comprehensive and integrated health care network in New Jersey.
During the 90-minute roundtable discussion, panelists addressed the use of artificial intelligence to improve care, the future of telehealth and telemedicine as well as the latest in at-home care, remote monitoring and wearable technology. They also discussed how an aging population will increasingly affect health care.
When it comes to artificial intelligence, panelists believe there are numerous uses within health care but agreed there must be guidelines.
“HMH really has been embracing AI technology for a number of years now … we have very strict and very robust governance policies to make sure that we manage AI and use the data in an appropriate way. We always believe there has to be human oversight in relation to it,” Young said.
“AI pulls information and draws conclusions. And where it pulls the information from – is the information correct and is it accurate? And then how applicable is that in relation to care that people receive?” he added. “We have about 300-plus use cases assigned to AI – streamlining administrative and clinical efficiencies, research and innovation, capacity management and burnout, deviation and disease detection.”
Lindgren said, “One of the questions for us is, as an executive team, what are the potential uses of AI? Where can it be most adopted and valuable to our industry and to our workforce? And what’s the return on investment there? AI can be a very sexy piece of equipment that you think could do anything, and maybe it can, but where are we really going to see the most bang for our buck in the utilization of AI? And I think that’s a decision executive teams really need to make.”
She explained, “We are interested in how AI can extend from the health care systems into adjacent systems of care. We provide behavioral health services, we provide services for aging individuals who are aging, so are there opportunities to take the benefits of that system and extend it? For example, we have a pilot program where we’re seeing can AI predict falls? It’s a very small pilot, but it aims to be utilized for preventative care and not just healthcare decision making.”
D’Angelo explained, “At NJIT, the university has made significant strides in AI adoption. Not only from a student facing perspective, but also faculty and as an organization and higher ed university. And then, looking at AI specifically in health care … we see EHR [electronic health records] systems implementing AI and their solutioning and models plugging into existing processes and protocols.
 New Jersey Innovation Institute recently launched NJII AI Lab, which will help small and medium-sized businesses with the adoption of artificial intelligence. – PROVIDED BY NJII
New Jersey Innovation Institute recently launched NJII AI Lab, which will help small and medium-sized businesses with the adoption of artificial intelligence. – PROVIDED BY NJII
“And you’re right, having the guardrails to make sure that we’re leveraging that appropriately, that we’re looking at that information in a very strategic way, looking at how we can have clinical decision making and leveraging those large data sets. Health care is data rich, taking those data sets and being able to have some predictive analytics, diagnostics, speed and accuracy, reducing some human error,” she said.
D’Angelo continued, “Everybody wants to hear how AI fits into their industry and into their workflow as an asset to the organization — not necessarily to replace people. Someone still needs to have governance and process over the output of AI. AI is not going to solve all of the problems, but it certainly is going to streamline some areas where you could do some quick analytics and some predictions, helping with chronic disease management and overall population health and management. We are seeing that quite a bit in all facets of health care.”
Making connections
Given the buzz around AI, panelists acknowledged there may be some misconceptions among the public about the technology.
D’Angelo said, “There’s a lot happening in health tech. Their records are made readily available to them through a variety of different mechanisms and portals, depending on a health system or provider practice. So, I think really educating the patient on incorporating AI as a best practice protocol to help the provider and facility achieve quality customer service to that patient is incredibly important.”
Replay: Trends in Health Care Panel Discussion
Click through to register to watch the full panel discussion!
“Patients are very much aware of their data more so today than I think ever before. So, how are we using that data? How are we helping them look at their diagnoses or their vital statistics over years of time? … How can we help them with their preventative health and wellness and how that health system or provider practice is leveraging those AI tools to really direct patient care? To me, that comes down to an educational process and getting rid of the stigma, perhaps, that comes with AI and how it really is a benefit to the provider to then help direct patient care and the outcome for the patient,” she explained.
Haddad echoed the sentiment, saying, “There is a role for AI in every piece of the business, be that in the network footprint, be that in research and development, be that in clinical studies or be that actually in the delivery of care … We are on a journey, so this is not a be all end all one widget or gadget at a time. This is really constructing an ecosystem that’s intelligent, that can evolve and more importantly, adapt to the workflows that health care professionals have.”
There is a role for AI in every piece of the business … We are on a journey, so this is not a be all end all one widget or gadget at a time. This is really constructing an ecosystem that’s intelligent, that can evolve and more importantly, adapt to the workflows that health care professionals have.
– Said Haddad, J&J MedTech Surgery, president
Young said, “I would say that there are clearly inroads being made in relation to the aggregation of all the data and then utilizing that information to improve personalized and equitable plans for patients. So, I think that is something that is evolving. But I think, again, you just need to make sure that what you’re using in the data and how it’s being aggregated and the source that it’s coming from is used appropriately.”
“But at the end of the day, I think it’s about aggregating all that data and that information that’s available and then making it a useful tool for physicians … It’s not the end solution. It’s a tool that doctors, nurses and health care providers can use to improve their efficiencies and their effectiveness,” Young said.
As for electronic health records, panelists said AI is already incorporated into systems and has been for a while.
D’Angelo said, “It maybe wasn’t in the form of an end user interface like ChatGPT, but health care facilities have been using predictive analytics for some time. I think it’s baked into a lot of these solutions. And the vendors are quickly trying to incorporate AI tools into a variety of different modules within the electronic health record.”
“And of course, this is a ripe space for entrepreneurs to develop solutions that embed AI to solve a problem for X. So, if you’re looking at possible sepsis, there are vendors out there that are coming up with algorithms to predict sepsis earlier,” she explained. “But it’s certainly intertwined within electronic health records and standalone third-party applications integrated to other systems. And it really touches a lot of the record, not only within the hospital health system, but outside of that, too.”
Managing risk
Young reiterated the need for “appropriate guardrails,” saying, “Because it is new technology, how it’s used, how are the patients protected, how is their information protected is the utmost importance of HMH.”
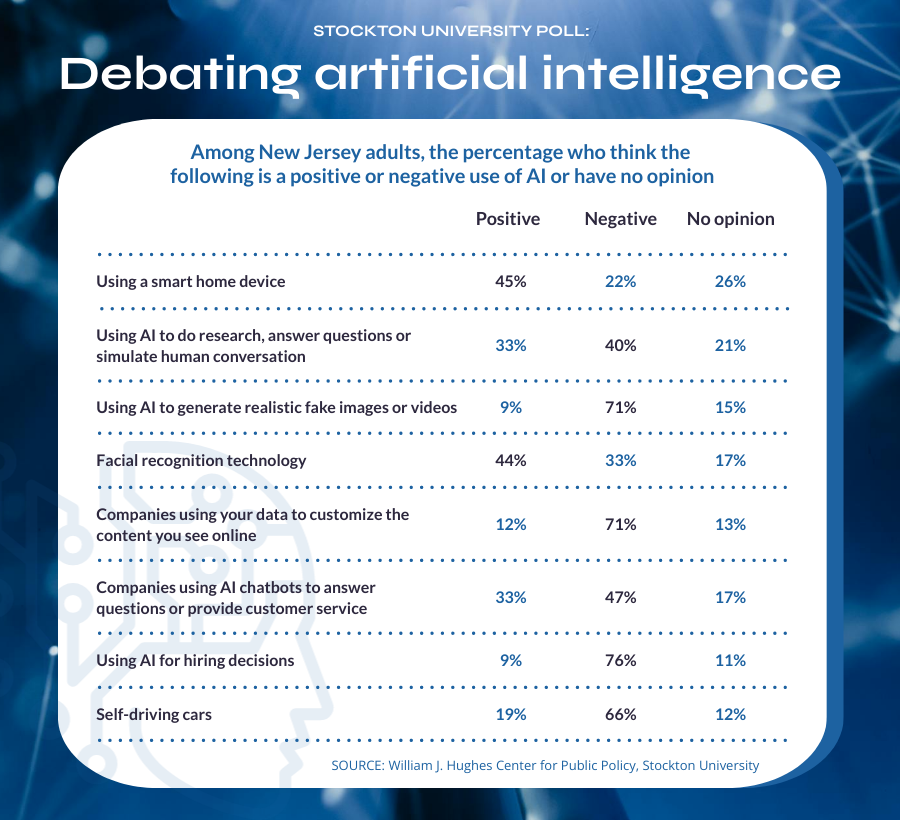 A March 2024 Stockton University poll gauged New Jerseyans’s concerns over the increased use of artificial intelligence. Click on the graphic for a closer view, and click here to read the full story. – INFOGRAPHIC CREATED IN PIKTOCHART
A March 2024 Stockton University poll gauged New Jerseyans’s concerns over the increased use of artificial intelligence. Click on the graphic for a closer view, and click here to read the full story. – INFOGRAPHIC CREATED IN PIKTOCHART
“Using the information to improve the quality of care and lower cost, I think AI has that as its expected outcome. But at the same time, there’s a lot of bad characters out there who can use AI in the wrong way. And so, in the health care field, we need to make sure that there’s a good governance structure, there’s an understanding, there’s a process, and that we put the patient’s privacy and their information of the utmost importance while also continuing to improve the quality of care and lowering costs,” he said.
“For us, we’re trying to leverage how can we utilize it to be maximizing the information exchange, maximizing wellness and preventative care for the patients, maximizing the information that the doctors get while protecting all those things,” said Young, who stressed, “It’s not as simple as just connecting and going. There’s a lot of thought and structure that needs to be put behind it.”
Lindgren noted, “The challenge, of course, for us is how we interact with other agencies and as we interact with other health systems, ensuring that what we are providing and what they’re providing to us matches those same guardrails and structures. AI is going to explode quickly from being within an organization to being within the whole ecosystem and we have to figure out how we’re going to manage that.”
Young agreed, saying that health care organizations must do their due diligence in evaluating potential partners. “Because you interface with that organization and if there’s a breach, all of the sudden it becomes your breach … For our organization, we have very strict guidelines … For our partners, we hold them to the same high standards that we have because there’s no going backwards in relation to data breaches or personal information and who we interact with as an organization. For us, we think it’s a critical audit,” he stated.
Lindgren commented, “We need to make sure that the health systems we’re working with have the same level of integrity and diligence around what they’re doing. And we find when we work at that, we continue to learn and improve and grow.”
She continued, “But, there’s a lot of education that needs to occur amongst all levels of folks in our organization and in the system around what it is, what we’re trying to accomplish, and how data breaches might look because they might look different. It’s not the same as leaving a chart out on a desk or dropping somebody’s name. It’s a very different type of thing. And helping people understand as we move into this new world, what are the risks and what are we really looking for?”
Hospital-at-home
For hospital-at-home programs – which enable some patients who need acute-level treatment to receive care at their homes, rather than in a hospital – wearable technology is “at the core of making it a success,” said D’Angelo. “There’s so much that goes into that, making sure that the systems are in place and really pulling family in as part of the process. We expect more for our parents and for aging communities. We want to keep them in the home and we want to keep them where it’s comfortable. And technology sits at the core of that — having the right tools and wearables to be able to do remote patient monitoring and also telehealth services and telemedicine,” she said.
As part of a newly launched program at HMH, the system moved 260 patients at Hackensack University Medical Center, Jersey Shore University Medical Center and JFK University Medical Center back home since the end of April, Young said.
 As part of a newly launched program at Hackensack Meridian Health, the system moved 260 patients at Hackensack University Medical Center, Jersey Shore University Medical Center and JFK University Medical Center back home since the end of April. Shown is the Hope Tower at JSUMC. – PROVIDED BY DEWBERRY
As part of a newly launched program at Hackensack Meridian Health, the system moved 260 patients at Hackensack University Medical Center, Jersey Shore University Medical Center and JFK University Medical Center back home since the end of April. Shown is the Hope Tower at JSUMC. – PROVIDED BY DEWBERRY
According to him, the initiative will expand to two-to-three additional facilities next year. “The feedback has been very, very positive. Reinfection rates are lower, readmission rates are lower,” he said. “It’s a scalable item. We believe this is a huge opportunity and we believe that is where the market is going … But we can’t do any of this without the physicians in the community supporting it.
“If we do this right, an individual doesn’t even need to go to a SNF [skilled nursing facility], because discharged right from the hospital for their home and they’re already in their home. So, there’s also a cost avoidance of care that wouldn’t necessarily need to be done. And then readmission rates are lower and infection rates are lower. There’s a lot of great reasons, but the idea about what we’re doing here as an organization, you’ve got IV antibiotics; infusion; medical management; laboratory services; physical, occupational, speech therapy; respiratory therapy, all these services that were being done in the institutions are now being done in the home,” Young said.
“And ultimately, our goal … is that when a paramedic goes out and sees a person, they have a physician with them on their iPad, they make an assessment, and we actually put the person right in their home. They don’t even go to the emergency room. That’s where we’re moving and that’s our future direction,” he stated.
According to Young, it took about six-and-a-half months to roll the program out in each hospital. “That included clinical protocols, the logistics and also educating the physicians as to how the program is, how we’re not going to do any harm, how it’s structured, what’s the backup, how do we handle all these issues? It’s a tremendous amount of work, but the success that we have is remarkable.”
“We’re moving to where I’d say the puck is going versus where the puck is, because our society is changing and not everybody wants to go into a hospital for their services. And that’s why we’re building very large ambulatory sites all over the state, because we’re trying to meet the patients where they are, which is where they live. And so philosophically, this is something we’re very committed to and something we’re very excited about,” Young said.
For companies like New Brunswick-based health giant Johnson & Johnson, the trend has implications for its operations, according to Haddad. “We are seeing a huge migration of surgeries out of centralized large hospitals to ASCs [ambulatory surgical centers] … across the country,” he said. “The implication for us is obviously our distribution model and how can we better support physicians as they do those kinds of surgeries outside of a traditional hospital setting. There’s a big implication for a company like J&J from the distribution perspective, from a support perspective, from a customer service perspective and a quality perspective.”
Wearable technology
D’Angelo said wearable technology, such as fitness trackers and ECG sensors, is “where you get significant adoption” from patients and consumers.
“They like being able to look at their app and see how many steps they’ve taken and monitor their heart rate. There’s a sense of collaboration and synergies now that the patient can have with a provider when it comes to the wearables and they’re not as scared about leveraging that data that they own and sharing that with their providers,” she said.
 Panelist Jennifer D’Angelo, chief operating officer & executive vice president of healthcare at New Jersey Innovation Institute D’Angelo said wearable technology, such as fitness trackers and ECG sensors, is “where you get significant adoption” from patients and consumers. – DEPOSIT PHOTOS
Panelist Jennifer D’Angelo, chief operating officer & executive vice president of healthcare at New Jersey Innovation Institute D’Angelo said wearable technology, such as fitness trackers and ECG sensors, is “where you get significant adoption” from patients and consumers. – DEPOSIT PHOTOS
D’Angelo continued, “With the adoption of wearables, it’s definitely based on the demographic and the use case of the wearables. I think that for a hospital at home use case where there’s wearables, that’s helping them stay and remain being treated in their home environment. So, there’s a higher adoption rate, preventative health and wellness in an aging retirement community, they’re excited to wear wearables to prevent physician visits.”
For an organization like Bancroft, Lindgren said wearables “hold incredible promise” to help individuals who “might not be able to communicate” because it can relay health care information to doctors.
“They might be able to tell if they have an irregular heartbeat, fever or if their blood sugar is spiking,” she said. “The other thing for our industry that’s really fascinating is the potential. These technologies may be pulled in order to predict psychiatric or behavioral events … For our individuals who are frequent utilizers of psychiatric crisis or ER utilization, being able to predict and intervene ahead of time holds a lot of promise for health care and better quality of life for those folks.”
As the U.S. population ages, the need to ensure elderly patients are receiving high-quality care is a top priority despite workforce shortages. “In 2015, 12% of the population was above age 60. By 2050, a quarter is going to be above 60. Delivery of health care is mostly consumed by that age group … In a setting like this, we recognize we have to be – or help our customers be – a lot more efficient in what they do and deliver care in a manner that contains a lot of the costs,” Haddad said.
“We understand the economics of this are challenging, and in our minds kind of focusing health care to a value-based health care delivery system is something that’s really important. It’s critical to do, but it requires us to look at the delivery of care a little bit differently,” he said.
 As the U.S. population ages, the need to ensure elderly patients are receiving high-quality care is a top priority despite workforce shortages. – DEPOSIT PHOTOS
As the U.S. population ages, the need to ensure elderly patients are receiving high-quality care is a top priority despite workforce shortages. – DEPOSIT PHOTOS
D’Angelo said, “We’ve been looking very closely at the senior living space, and it’s an industry that’s really ripe for disruption and changing their philosophy … Unfortunately, in that space, it’s not as interoperable as it is on the acute side of the house. So, we’ve been looking at some strategy services to help these providers that are working in senior living – nursing home situations, assisted living facilities – and how do we help them bridge some of the gap and connect that continuum of care?”
She went on to say, “We’ve been doing a lot and have formed this provider collaborative that we help support. We’re seeing a lot of disruption in this space and try to help support those providers and organizations that really could use some additional help and resources where they don’t have robust IT teams, cybersecurity teams, and some of those services that are in the bigger health systems. We see a lot happening in that space.”
Young recalled, “About five years ago, I talked to [Hackensack Meridian CEO] Bob Garrett and we had a discussion with the board about New Jersey’s aging population. It’s growing significantly, not just here in New Jersey, but everywhere in the country. And we decided we wanted to create a new Medicare Advantage program called Braven Health. It’s the third largest individual MA program in New Jersey and a partnership with HMH, with Horizon and Robert Wood Johnson … In three years, we’ve grown it to almost 50,000 members.”
“It’s a different kind of company. The concept is that we can work closely with the payor in this situation to improve the quality of care of senior citizens. And it’s about sharing data, it’s about getting claims information, it’s feeding in our clinical information, and by using that information in a way and making it useful data so that when that senior citizen goes in to see the doctor, they already know all the care gaps,” he said. “ … All that information is there so that the patient is treated in a way which is using data to allow them to improve the quality care that those individuals have … So, we are all in on that, and we own 35% now. It is statewide, and we’re very proud of the success of that program.”
Interoperability
Panelists also spoke about how interoperability can be used to reduce costs and enhance patient experience.
Haddad cited the World Health Organization’s findings that up to 40% of global health care spending is wasted through inefficiency. He said, “Interoperability takes a knife to that and I think it’s really important.”
D’Angelo said, “As we foster statewide interoperability within health system interoperability … having those systems connected and having that data accessible reduces unnecessary possible tests, unnecessary documentation or decreases the ability to say ‘Oh, we missed ordering a test or we missed a step in the process.’ So, supporting interoperability from that perspective definitely has a cost reduction.”
“Most people ask and want to know very specifically, where do we reduce the cost? Well, it really depends on the organization’s adoption of interoperability and what they actually do with those messages that they receive for event notifications. How do they follow up with patients and providers? How do they incorporate that in the day-to-day workflow to really streamline the process of the data they’re receiving and making those action items?” she explained.
Young added, “The sooner you identify an illness and start treating that illness, the better — and the less cost it produces. And the ability to identify those issues, those chronic illnesses early and start treating the patient is about a holistic view of that whole person. It’s not just that they have congestive heart failure, what’s caused it? What’s caused the diabetes? What’s their diet? What’s their exercise? And so, to the extent that you can intervene early as possible, I think the implications have significant financial implications going forward.”





